Oral Contraceptives Side Effects

Dr. Álvaro Monterrosa Castro, MD
dbecause oral contraceptives can supply a greater or lesser amount of hormones to which the body is accustomed. Some users will present some side effects, which generally occur in the first two or three cycles. (1.51).
In general, some of these symptoms occur in up to 25% of users when they receive their first cycle. But they decrease to the point that only 5% present them beyond the 3rd cycle.
On many occasions, users attribute symptoms to the tablets that are not actually caused by them. The side effects that are related to oral contraceptives are indicated in the Table No. 2.
TABLE Nº 2: Side effects of oral contraceptives
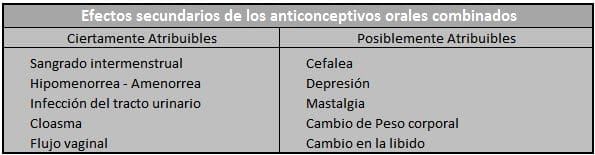
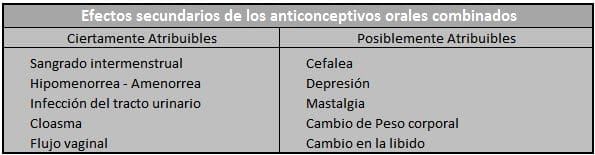 Porte WC, Waife RS, Holtrop HR. (19).
Porte WC, Waife RS, Holtrop HR. (19).
Health personnel should listen to these complaints, be understanding and reassure the user. Since these side effects are usually easily managed and resolved (10).
The most common adverse effect caused by monophasic or triphasic combined oral contraceptives is headache (0.6 – 13%). Breast tension occurs in 0.5 – 12%. Nervousness 0 – 8.4%, nausea 0 – 6%. Depression 0 – 4% and vertigo 0 – 3%.
Additionally, weight gain and increased blood pressure are generally occasional and acne occurs in 0.3 – 5.8% of users. The incidence of these adverse effects after three or four cycles of taking the pill is similar to that before using them. (7.21).
Intermenstrual bleeding and spotting
Irregular or intermenstrual vaginal bleeding and spotting or dripping. They are part of the most common side effects and are usually reasons for abandoning the use of oral contraceptives, if the user has not been properly informed. (30,42).
First, intermenstrual bleeding and spotting during the first cycles of microdose contraceptive use (7.17). It is a common event that should not be a cause for alarm. Which is because by administering contraceptive steroids at low doses to reduce side effects and maximize safety, complete cycle control is not achieved. (30).
Second, combined oral contraceptives that include 20 ug of ethinyl-estradiol have more irregular cycle control than 30 ug oral contraceptives. (25). Intermenstrual bleeding is usually more common in women with a history of irregular bleeding. (7). Irregular use of contraceptive tablets is usually the cause of poor cycle control. Increasing the incidence of intermenstrual bleeding and spotting (17).
Third, smoking users experience between 20 and 90% more spotting and intermenstrual bleeding than non-smokers. Weight or age have no influence on bleeding irregularities. Rosember stated at the IX International Congress of the Association for the Advancement of Contraception, held in Guatemala in 1995.
Additionally, if the bleeding is heavy or persistent, the user should be carefully evaluated. And look for the existence of some gynecological pathology that explains said bleeding.
On the other hand, intermenstrual bleeding, also called leak bleeding, is bleeding that warrants protection. It is produced by relative estrogen deficiency and progestin-induced decidualization. (42.17).
The endometrium is flat, thin, which makes it fragile and prone to disintegration and causing irregular bleeding. This manifestation often disappears spontaneously in the next cycles (30).
Sometimes the bleeding can be so little that it does not require protection. It is called Spotting or staining or dripping (17,30,42). Which can occur in the first months of using the contraceptive (Four. Five).
Previously, it was suggested to take two tablets of the contraceptive preparation daily or even resort to a macrodose preparation. We should not allow users to take two tablets daily for more than one cycle nor should they continue using macrodoses.
Finally, the user will be reassured. Allowing the symptom to improve spontaneously or managing it by switching to another microdose preparation. And if it still persists, a very rare situation. They will be stopped and you will switch to another non-hormonal method of family planning.
Oral contraceptives containing Gestodene appear to control the cycle more effectively than other latest generation progestogens. (38.64).
These two bleeding modalities (17,65) tend to be much more frequent with triphasic combined oral contraceptives than with monophasic ones. And they are due to the tissue disintegration that the endometrium experiences as it adapts. From a greater thickness in the cycle without hormonal contraception to a thinner state. Induced by the low concentration of the synthetic steroids present in the pill (21.42).
Due to the discomfort caused by intermenstrual bleeding. The effectiveness in controlling the cycle is evaluated in different commercial preparations. (47.65).
In users of Tri-Cilest ® In the first cycle, leak bleeding occurs in 6.8% and spotting in 14.8%. Between cycles 13 and 24. Bleeding from leakage decreases to 2.4% and spotting decreases to 5.4%.
(Read Also: Benefits of Oral Contraceptives)
Hypomenorrhea and Amenorrhea
Hypomenorrhea is a consistent event in patients receiving microdose oral contraceptives. Andolsek (42) evaluated a triphasic regimen of Norgestimate and Ethinyl-estradiol. Noting that minimal and insignificant changes occurred in bleeding volume. And the average duration of menstruation decreased from 5.58 days in the first cycle to 5.07 days during cycles 13 – 24.
The low estrogenic content present in the tablet does not have enough power to grow the endometrium. And when a predominance of the progestogenic effect occurs, endometrial flattening and atrophy occurs.
The loss of the little endometrial tissue will manifest clinically as hypomenorrhea. A condition that in turn will bring about a beneficial consequence of reducing the incidence of iron deficiency anemia.
This effect on the endometrium is reversible upon resumption of ovarian function. By stopping the use of oral contraceptives, their growth and development will be restored.
There is no evidence that oral contraceptives cause secondary amenorrhea. The incidence of amenorrhea with the use of the pill is 0.8%. Especially when it occurs, it usually generates a lot of anxiety and uncertainty due to the fear of pregnancy.
If these types of events occur, the oral contraceptive should be discontinued and the patient switched to a non-hormonal method of contraception. 80% of patients will regain normal menstrual function within three months. And after one year, 95-98% will have normal ovulations.
This tendency toward hypomenorrhea is observed even in patients with uterine myomatosis. In which the days of menstrual flow are usually reduced (66).
Urinary tract infection
Porter et al. (19) they cite studies carried out by the Royal College Of General Practitioners and another by Walnut Creek. They claim to have found a significant increase in the risk of urinary infections among users of all ages, compared to non-users.
Both investigations estimate that these findings are due to increased sexual activity.
Vaginal discharge
High-estrogen concentration oral contraceptives are associated with an increase in the frequency of vaginal colonization by Candida. But these findings have not been confirmed in users of microdose combined oral contraceptives. (67).
In an assessment carried out by Spinillo and Col (67). They found that the pill does not influence the occurrence of sporadic fungal infection. But they are a significant risk factor for recurrent candidiasis.
The frequency of recurrent vaginal candidiasis is small and there are multiple factors that can influence its presence.
The mechanisms responsible for the association between microdose oral contraceptives and recurrent candida infection are evidently not known. It has been suggested that reproductive hormones may affect local cell-mediated immunity.
Spinillo and Cabbage (67) advise that the small proportion of women affected by recurrent vaginal candidiasis. Oral contraceptive users. They may benefit from stopping the pill.
Chloasma
It is an increase in the pigmentation of the skin on the face, similar to the pregnancy spot. Chloasma is related to estrogen levels and was much more common with the old macrodose preparations.
Its appearance can be prevented by avoiding repeated exposure to sunlight. It should be noted that it may take a long time to disappear. Or it may not even disappear completely.
Headache
Oral contraceptive users who present with persistent headache. They must suspend the method and be evaluated to rule out neurological pathology.
Migraine is a strong, throbbing headache. Generally preceded by visual disturbances and accompanied by nausea, which is often relieved with sleep. Produced by spasm of blood vessels and constitutes a formal contraindication to the use of oral contraceptives (19).
If the headaches are interpreted as being of psychosomatic origin. Caused by psychological or emotional tension and the Neurology assessment is normal. The method can be continued with formulas with very low estrogen concentrations. (30). For example Ethinyl-estradiol at 20 ug.
Depression
Mental depression is a common event. Being difficult to study its relationship with the use of oral contraceptives.
It has been suggested that the pill induces pyridoxine (vitamin B6) deficiency and interference with tryptophan synthesis. Which alters some metabolic processes, disturbing normal neurological function and producing depressive symptoms. (19).
Research is conflicting on oral contraceptive use and depression. However, it seems prudent to stop the pill if mental depression occurs.
Mastalgia
Users with persistent breast hypersensitivity. They can be switched to oral contraceptives that contain lower doses of estrogen or another type of progestin (1). Like Levonorgestrel.
Some British studies have reported that oral contraceptives with very potent progestogens. For example Levonorgestrelproduce fewer breast symptoms (30.68).
Body weight changes
Permanent weight gain is usually an anabolic response to sex steroids. Androgenic effect caused by the progestin. Event that was much more marked with the old macrodose pills.
The new microdose oral contraceptives and especially those that include the latest generation progestogens. They have minimal effect on carbohydrate metabolism. Reduced to zero androgenicity and practically no effect on the body’s metabolism (6.69).
Weight gain during the first cycle of pill use is often attributed to water retention caused by estrogen.
Libido changes
There is nothing more subjective in the lives of couples than sexual desire. Comparative studies of the frequency of sexual intercourse and orgasm, before and after the use of oral contraceptives, have not revealed differences.
As a result, some patients may experience an increased sexual desire. What can be produced by the disappearance of the fear of unwanted pregnancy (19).
In addition, the decrease in testosterone, produced by the latest generation Gonans. It would cause decreased libido in users of pills containing these progestogens. (6).