Oral Contraceptives in Women Over 35 Years

Dr. Álvaro Monterrosa Castro, MD
ANDThe climacteric is usually considered a prolonged period of a woman’s life and Ronald Bossenmayer (193) It is considered to start at 35 years of age. The climacteric is divided into three phases: Pre-menopause, menopause and post-menopause.
In the period between 40 and 50 years of age, ovarian function decreases. Fertility decreases and there is progressive atrophy of estrogen-dependent tissues. (35).
This decade is usually symptomatic for many women. Premenstrual syndrome intensifies, heat waves appear. Dysmenorrhea returns, changing or out of control moods are established. Menstrual cycles become unpredictable and menstrual periods become abundant or prolonged.
(Read Also: Emergency Contraception)
This symptomatology is usually intolerable and adversely affects the woman’s life.
William Beck Jr. (87) ruling that a safe, effective solution for many of these symptoms in healthy women, not hypertensive or smokers, at risk of pregnancy. It is the use of microdose oral contraceptives.
Additionally, the pill improves hypotrophic vaginitis. Apparently they partly prevent the loss of bone mass that begins after the age of 35 and partly prevent the decrease in skin collagen.
The 1995 IPPF International Medical Advisory Group statement (194). Consider that women over 35 years of age make up at least 20% of contraceptive users. This age group requires special attention since pregnancy in these women can entail greater risks for both the health of the mother and the baby. (87). Fertility control during the climatrium years is highly recommended (35).
Furthermore, among them there is usually a higher incidence of obesity, diabetes, high blood pressure and even smoking. Characteristics that affect when selecting the contraceptive methodology. All contraceptive methods should be considered, a comprehensive evaluation performed discussing benefits and risks.
It is important to inform about definitive surgical methods such as salpingectomy and vasectomy. Voluntary surgical contraception may be considered the best method for some well-informed couples. Which, by the way, is the method that is most popular in this age group. The termination of fertility is very likely, as the couple considers their reproductive desire completed. Be the target of older couples (194).
The use of the pill in women under 35 years of age decreased significantly in the seventies, when the association of the use of oral contraceptives with cardiovascular pathologies was reported. (195).
Epidemiological observations now indicate that the excess risk of vascular disease is limited to users who smoke. And age alone may not be a risk factor (169).
Therefore the use of oral contraceptives is increasing among older women. The reduction in hormonal content and the low adverse effect on lipids of the new progestogens are two events to consider. (195).
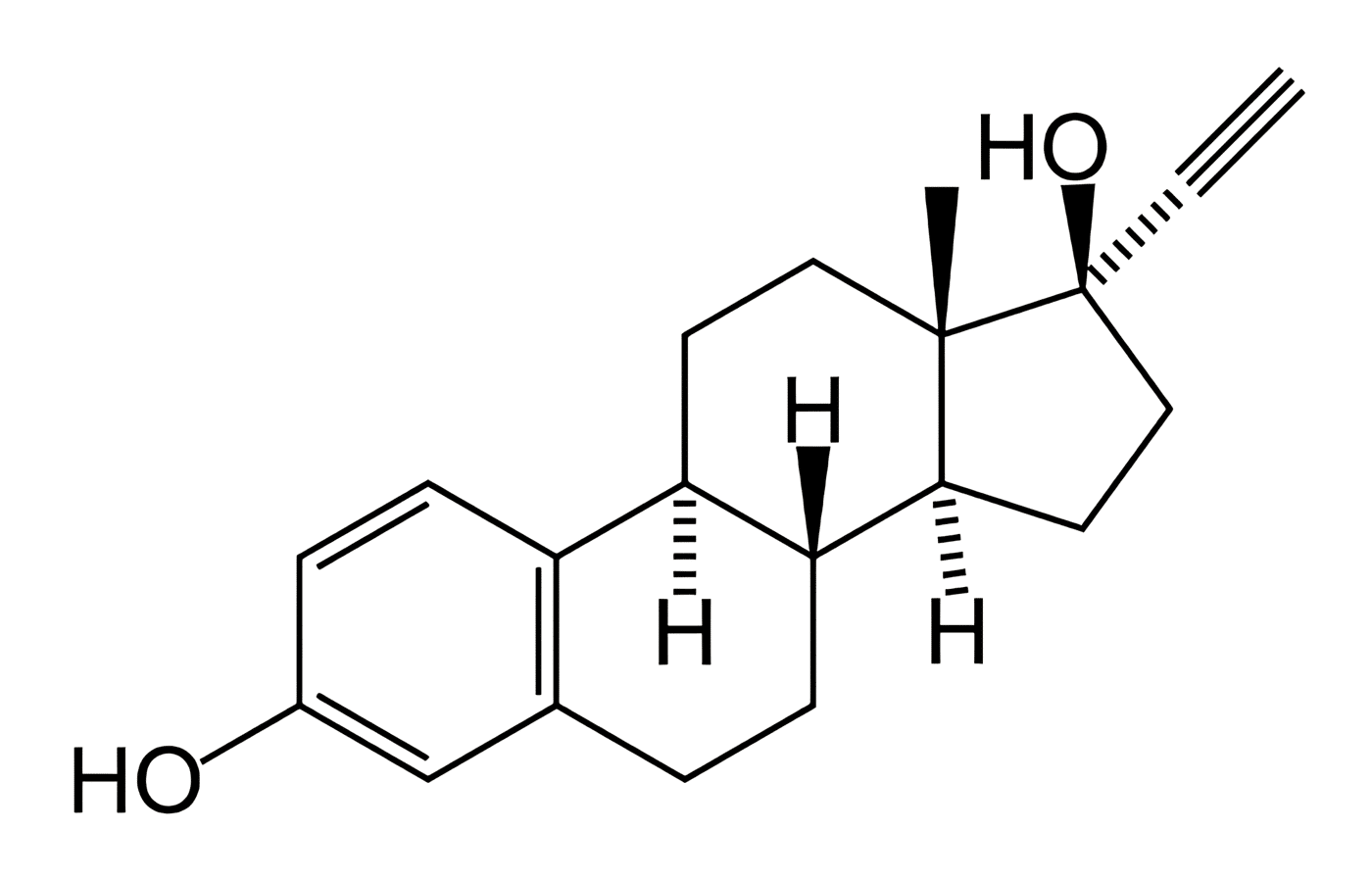
Microdose oral contraceptives, combined, monophasic or triphasic, can be used in women over 35 years of age. (193,194). In recent years, pills containing metabolically neutral progestogens, such as Desogestrel, Norgestimate or Gestodene, have been preferred. Many triphasic drugs are recommended, which usually provide the same concentration or 8% more estrogen, but up to 40% less gestagen. (193).
There is evidence that the cardiovascular risk is minimal in these women. As long as they don’t smoke (69,169). And they do not have other risk factors such as high blood pressure, obesity, a history of alterations in the coagulation system. Thromboembolic phenomena or cerebrovascular accidents or diabetes. Sedentary lifestyle, hypercholesterolemia or family history of myocardial infarction at young ages (194). If any of these conditions are present, oral contraceptives should be contraindicated in women over 35 years of age.
Progestogen-only oral contraceptives (minipills). They offer the advantage of being free of estrogen-related side effects and may be indicated when there is a formal contraindication to the use of estrogens. (193). But for causing alterations in menstrual function. They could hide or simulate bleeding produced by those gynecological pathologies that occur at these ages.
If highly effective contraception is not used, maternal mortality is 22.6 per 100,000 women per year.
This proportion is reduced to a third (7.1) when oral contraceptives are used in non-smokers. If you are a smoker, the risk of death increases 8 times (58.9) by using pills. But even so, this mortality is lower than maternal mortality in women over 40 years of age who become pregnant due to not using any contraceptive method. (193).
Fertility is practically lost about 5 years before menopause. And the possibility of pregnancy is very low in women with clear perimenopause signs such as oligomenorrhea and hot flashes. However, there is difficulty in precisely specifying the moment in which a woman’s fertile capacity disappears. (69).
Oral contraceptives can be used until the user experiences episodes of amenorrhea. (35). FSH and LH will then be determined. If the levels are compatible with a post-menopausal state, oral contraceptives are terminated and hormonal replacement therapy is changed. (87).
Another alternative is that around the age of 40-45, the method is suspended for a period of six weeks. A barrier method is used in this period of time and FSH and LH titers are defined. If they are increased, treatment will be changed to hormone replacement therapy. (193,195).
The US Food Drug Administration (FDA) recommends that it is not necessary to indicate a maximum age limit for ordering oral contraceptives to a normotensive woman who does not smoke and who does not present a risk for cardiovascular disease. (195). This practice is also spreading in Great Britain. (62,64).
Desogestrel combined with 20 Ug of Ethinyl-estradiol can be an interesting alternative for pre-menopausal users. (35.39).
First, this combination was used by Trossarelli et al (35) in 58 healthy women between 35 and 49 years old.
Observing significant statistical improvement in climacteric symptoms such as hot flashes, insomnia, arthralgias, palpitations, paresthesias, nervousness, fatigue and dizziness.
Furthermore, no pregnancies occurred during the year of follow-up. Finally, there was adequate cycle control and good tolerance. Without significant changes in blood pressure and body mass index.